DR DAN REARDON LIFESTYLE MEDICINE CONSULTANT
LIFESTYLE MEDICINE CLINIC
Clinician-led medication review and deprescribing where appropriate—plus metabolic health optimisation for long-term maintenance and longevity.
Deprescribing pathways • Metabolic health • Weight maintenance • Longevity
Clinician-led • Strength-first • Data-led • No gimmicks
Clinical appointments are provided by CQC-registered Sutton Medical Consulting
NHS A&E Doctor • Health Tech Founder • Medical Advisor
CORE SERVICES
Two pathways: medication strategy and metabolic performance.
TESTIMONIALS
Trusted by high performers — grounded in clinical judgement.
AS SEEN / SPOKEN AT
Health 2.0
Buzzfeed
The Doctors
Upgrade
GCN
Bulletproof
Selected appearances and talks across health, performance, and technology. Click to read more
DEPRESCRIBING PHILOSOPHY
Deprescribing is the easy part. Staying stable afterwards is the work.
Medical Review
Clarify indication, current benefit, and risk
Identify interactions and “medication load”
Shared decision-making, not ideology
Deprescribing Strategy
Step-down planning where appropriate
Symptom monitoring and contingency rules
Coordination with your GP/specialist when needed
Lifestyle & Performance Rebuild
Strength-first body composition strategy
Appetite/satiety structure and food environment design
Sleep, stress physiology, and long-term maintenance systems
DEPRESCRIBING PATHWAYS
Choose your starting point — each has a different rebound pattern.
CLINICAL PROCESS
Assess → Stabilise → Plan → Taper / Adjust → Maintain
-
We review your history, goals, current medication list, and previous attempts. We map the likely rebound points and decide what success needs to look like for you.
-
Before changing anything, we build a stable baseline: nutrition structure, strength plan, sleep anchors, and symptom tracking. This reduces noise and improves decision-making.
-
You get a personalised plan based on risk/benefit: what to continue, what to adjust, and what may be reduced (where appropriate). Clear monitoring targets and check-in points.
-
Step-down is gradual and responsive, with symptom tracking and decision rules. We go slower if needed and coordinate with your GP/specialist where appropriate.
-
We lock in maintenance: habits, environment design, relapse prevention, and follow-up. The goal is stability without white-knuckling.
Medication changes are always individual and should never be done abruptly.
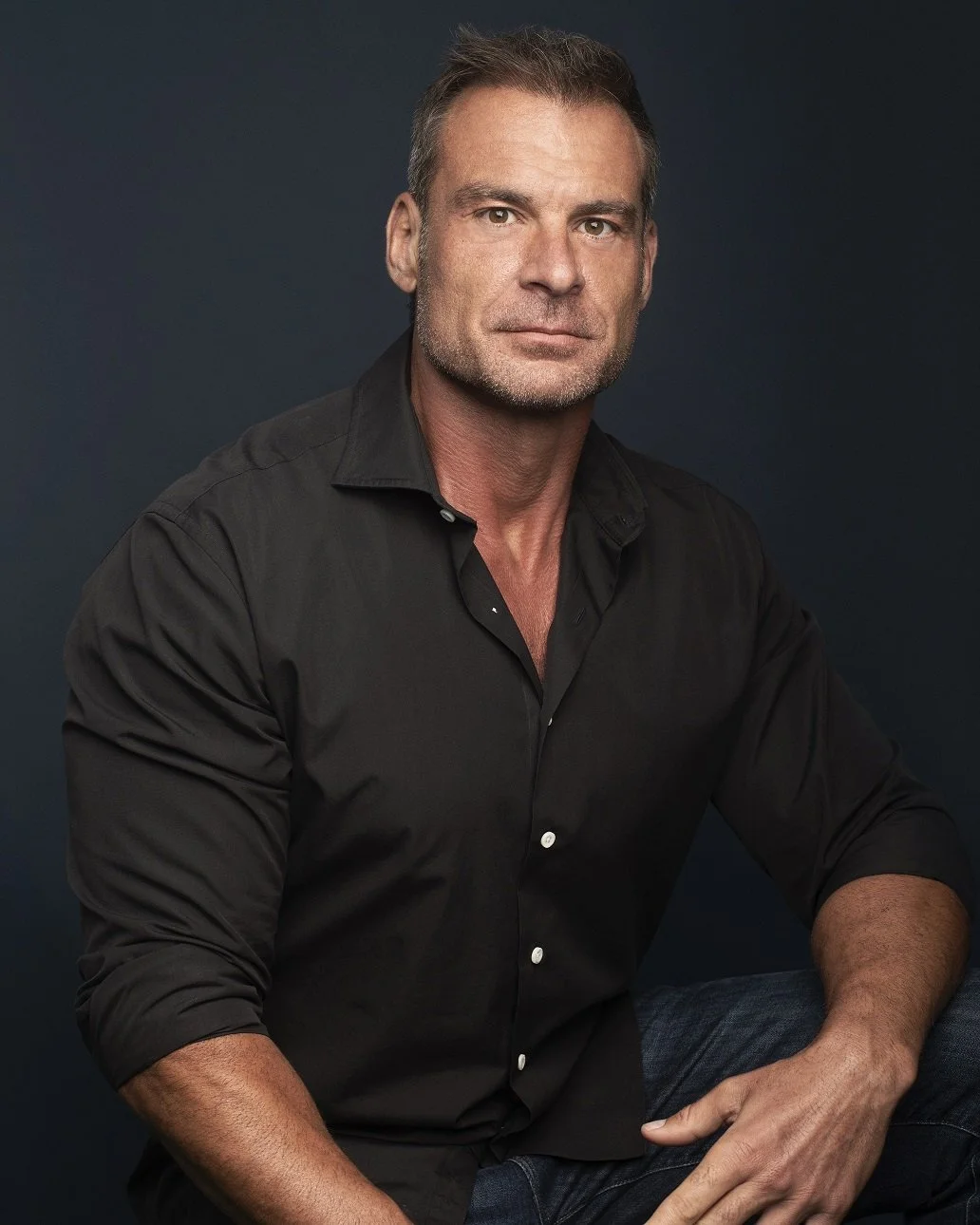
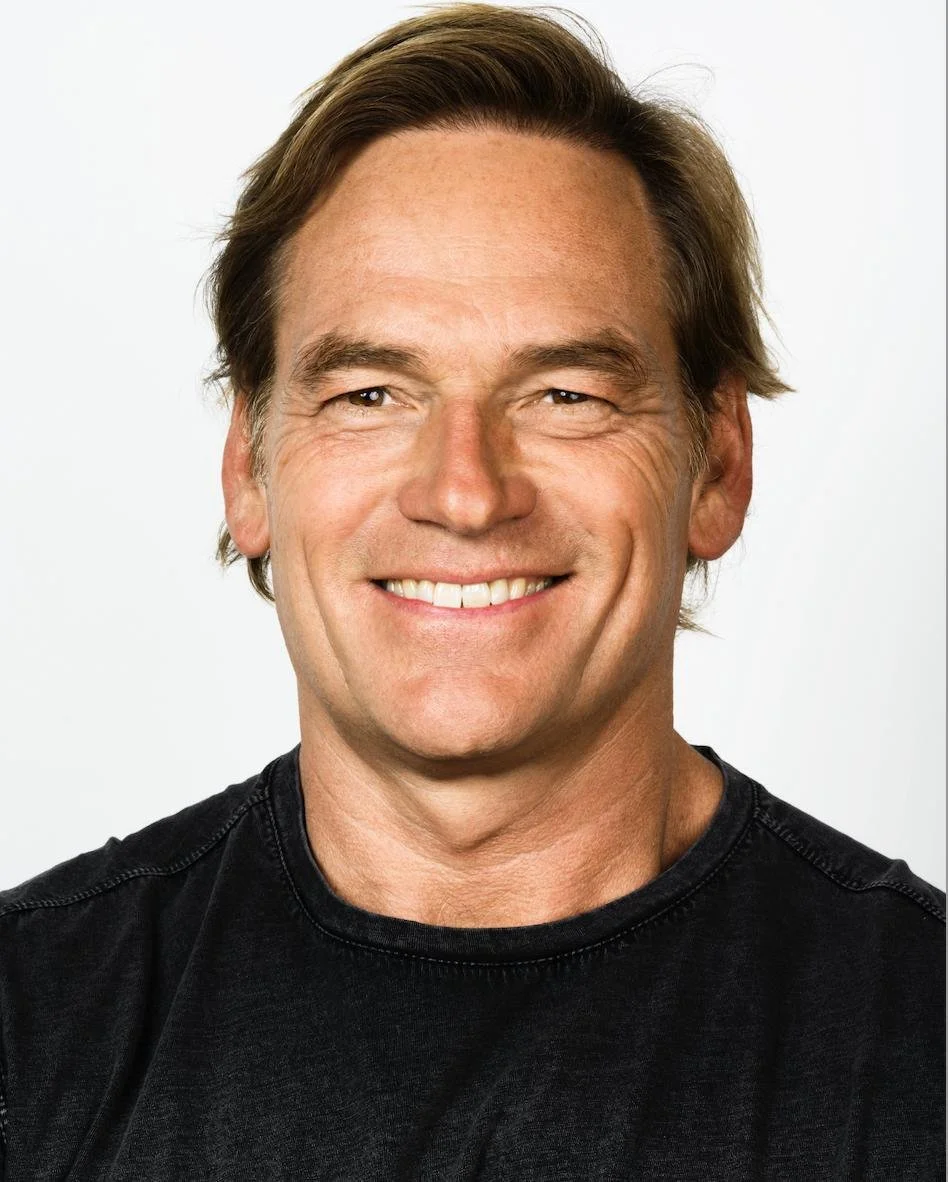
CLINICAL LEAD
A doctor who understands physiology — and what people can actually sustain.
I continue to work in the NHS A&E and privately specialise in the gap between intention and reality—building systems that make change stick. My background spans clinical medicine, sports performance, education, and health technology, translating physiology into outcomes you can repeat.
NHS A&E doctor — frontline clinical reality
Founder + medical advisor — systems, strategy, outcomes
Public educator — media, podcasts, international speaking
PATIENT FIT
If any of these are you, this clinic is built for you.
Includes GLP-1/GLP-1+GIP therapies, statins, antidepressants, PPIs and antihypertensives — where deprescribing is appropriate and safe.
FAQ
The practical questions — answered clearly.
-
No. We review indication and risk/benefit. Sometimes the right answer is to continue, adjust, or deprescribe—case by case.
-
Yes, where appropriate. Some plans work best in shared care.
-
No. Many medications require gradual tapering and monitoring. Never stop abruptly without clinical advice.
-
GLP-1 exit is the flagship pathway, but the clinic covers multiple deprescribing pathways.